

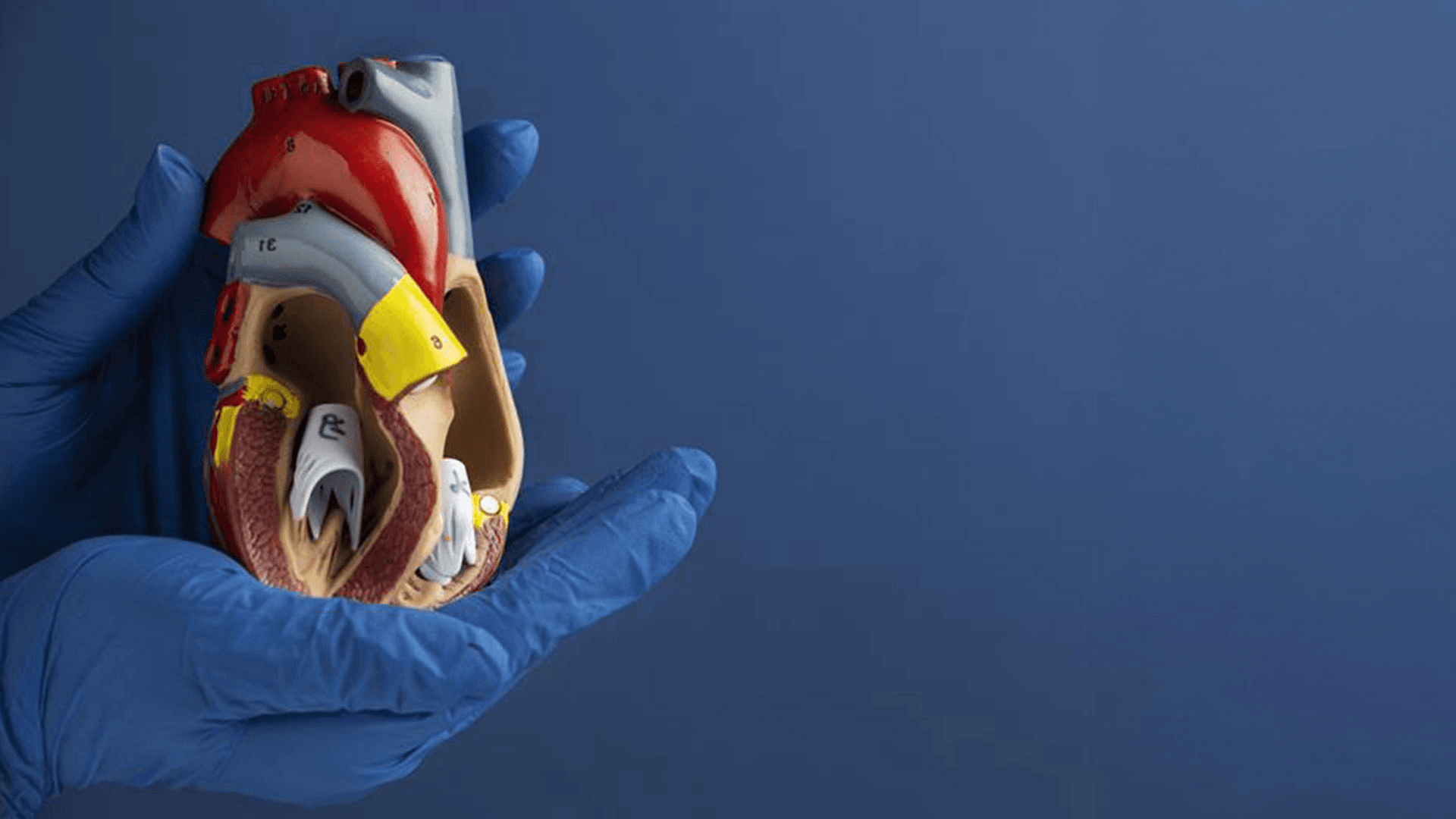
Cardiology
No Referrals Required
Cardiology Services

Common Heart Conditions
Hypertension (High Blood Pressure)
Heart Failure
Dilated Cardiomyopathy
Heart Valve Disease
High Cholesterol
Arrhythmia
Risk of Heart Disease
Cardio-Oncology
Atrial Fibrillation
Coronary Artery Disease
Hyperlipidaemia
Angina
Heart Murmur
Inherited cardiomyopathy conditions

When to see a cardiologist?
Chest Pain
Dizziness
Palpitations
Loss of Consciousness
Long Covid Symptoms
Shortness of breath

Diagnostics & Imaging
Echocardiography
Contrast Echocardiography
Transesophageal Echocardiogram
Cardiac MRI
Cardiac CT
Ambulatory ECG
Exercise Stress Echocardiography
Dobutamine Stress Echo
Bubble Echo

Interventions & Management
Pacemakers
Implantable cardioverter defibrillator (ICD)
Preventive Cardiology
General Cardiology
CRT Cardiac Resynchronisation
Leadless Pacemakers
Conduction System Pacing
Cardiac ablation
Cardiac Screening
Cardiology Consultation Options

In-person Cardiology Appointment at LIPS Healthcare
You can see your Cardiologist face-to-face in-clinic for a consultation

Online Cardiology Appointment
You can book a virtual Cardiology consultation.
Book an appointment
This is a provisional booking. A member of our team will contact you shortly to confirm and arrange the details of your visit.
This is a provisional booking. A member of our team will contact you shortly to confirm and arrange the details of your visit.

Cardiologists Around London

FAQs
You can book an appointment through any of the following options:
Email us at info@lips.org.uk
Call us at +44 (0) 207 164 6114.
Book directly through our website.
Self-Pay
Booking Online:
Debit or credit card (Visa & Mastercard)
Apple Pay or Google Pay
Booking Over the Phone:
A secure online payment link, shared by the medical assistant.
Alternatively, you can provide your card details over the phone to our medical assistant for a secure one-time card payment.
Insured:
You must provide the following details at the time of booking, either online, over the phone or via email:
Insurer name
Authorisation code
Membership number
Hypertension, or high blood pressure, is a condition where the force of the blood against the artery walls is consistently too high. It often develops over time and may not cause noticeable symptoms. If left untreated, it can increase the risk of serious health problems like heart disease, stroke, and kidney damage.
Yes, high blood pressure can cause dizziness, particularly during a hypertensive crisis or as a side effect of certain blood pressure medications. It may also affect blood flow to the inner ear, which helps control balance. If dizziness is sudden or severe, seek medical attention.
Heart failure doesn’t mean your heart has stopped working, it means your heart isn’t pumping blood as well as it should. When this happens, your body may not get enough oxygen and nutrients to work properly. You might feel tired, short of breath, or notice swelling in your legs or ankles.
It’s a long-term condition, but with the right treatment and lifestyle changes, many people live well with heart failure and keep it under control.
Heart failure usually happens when something damages or weakens the heart over time. Some of the most common causes include:
High blood pressure – makes the heart work too hard, causing it to weaken.
Heart attacks – can damage the heart muscle.
Heart valve problems – can affect blood flow and strain the heart.
Irregular heartbeats (arrhythmias) – can make the heart less efficient.
Diseases of the heart muscle (cardiomyopathy) – sometimes genetic or caused by infections, alcohol, or drug use.
Other health issues like diabetes, obesity, and thyroid problems can also play a role. Over time, these conditions make it harder for the heart to pump blood properly.
Congestive heart failure is usually described in four stages (A to D). These stages help doctors understand how advanced the condition is and guide treatment. Here’s a simple breakdown:
Stage A – At Risk
You don’t have heart failure yet.
But you have risk factors like high blood pressure, diabetes, or a family history of heart problems.
Goal: Prevent heart failure from developing with healthy habits and possibly medications.
Stage B – Early Heart Damage
Your heart has some damage or changes, but you don’t have symptoms yet.
Maybe you've had a heart attack or tests show your heart isn't pumping quite normally.
Goal: Start treatment early to stop it from getting worse.
Stage C – Symptoms Appear
You’ve been diagnosed with heart failure.
You may feel tired, short of breath, or notice swelling in your legs or ankles.
Goal: Manage symptoms and improve quality of life with medications, lifestyle changes, and regular follow-ups.
Stage D – Advanced Heart Failure
Symptoms are more severe and ongoing, even with treatment.
You may feel breathless at rest or have frequent hospital visits.
Goal: Specialized care, possibly including advanced therapies or procedures.
One key sign that heart failure may be getting worse in older adults is increasing shortness of breath, especially during everyday activities, or even when resting or lying down.
Other warning signs to watch for include:
Sudden weight gain (from fluid buildup)
Swelling in the legs, ankles, or belly
Feeling more tired or weak than usual
Coughing or wheezing, especially at night
Feeling confused or having trouble concentrating
If any of these symptoms appear or get worse, it's important to contact a healthcare provider right away. Catching changes early can help prevent serious complications.
Yes, you can live with heart failure. While it’s a long-term condition, many people manage it well and continue to live full, active lives.
The key is taking care of your heart every day. That means following your doctor’s advice, taking medications as prescribed, eating a heart-healthy diet, staying active, and keeping an eye on symptoms. Regular check-ups help your healthcare team catch any changes early and adjust your treatment if needed.
With the right care and lifestyle, heart failure doesn’t have to stop you from doing the things you enjoy.





